Microwave Ablation Fibroids Treatment In Malaysia Selangor Penang Johor
Microwave Ablation Fibroids Treatment In Malaysia Selangor Penang Johor
Microwave Ablation Fibroids Treatment In Malaysia Selangor Penang Johor
Microwave Ablation Fibroids Treatment In Malaysia Selangor Penang Johor
Microwave Ablation Fibroids Treatment In Malaysia Selangor Penang Johor
Microwave Ablation Fibroids Treatment In Malaysia Selangor Penang Johor
Thermal ablation techniques are increasingly used for the treatment of symptomatic uterine fibroids. Thermal protection of myometrial tissue adjacent to the fibroid from ablation is critical to maximally preserve the uterus. This study presents a bench top experimental setup, using ex vivo bovine muscle as a surrogate tissue, for evaluating collateral thermal damage in tissues during fibroid ablation. The study reports on the effect of applicator insertion angles (67.5° and 90°) into a mock fibroid on the efficacy of treatment. 6 experiments were performed (3 for each insertion angle) with 30 W applied power at 2.45 GHz. The heating duration was restricted to the time at which a thermal dose of 10 cumulative equivalent minutes at 43 °C (10 CEM 43) was accrued at the boundary of the mock fibroid. Results showed that the volume of ablation inside the mock fibroid dropped considerably from 66% to 17% when the applicator insertion angle was changed from 90 o to 67.5 o , suggesting that insertion angle plays an important role during microwave ablation of fibroid. The proposed setup provides a method for validating computational models for accurate and safe delivery of ablation to target tissues in fibroid treatment.
Microwave Ablation Fibroids Treatment In Malaysia Selangor Penang Johor
Symptoms of Fibroids & Adenomyosis
Not all women with fibroids have symptoms, women who do have symptoms often find fibroids or adenomyosis hard to live with. The symptoms are also related to their location in the uterus (we will talk about this in the next section!). The main symptoms are:

- Heavy and painful menstrual bleeding
- Menstrual periods lasting more than 1 week
- Irregular bleeding between your periods

Swollen belly that look like pregnant

Feeling of fullness in the pelvic area (lower stomach area)

- Frequent urination
- Difficult emptying the bladder
- Constipation

Lower back pain

Difficult to get pregnant

Complications during pregnancy and labour
Where Can Fibroids Grow?
There are many different types of fibroids and each are categorized by their location in the uterus. However, only certain types of fibroids are suitable for Microwave Ablation Treatment.
🟣 Submucosal Fibroids: Develop under the lining of the uterus cavity. When it grows, it will increase the size of the uterus cavity and block the fallopian tubes, which can lead to complications with fertility. Associated symptoms include excessive periods bleeding and prolonged menstrual cycles. These symptoms can cause the passing of clots and frequent soiling, which can take its toll on your everyday lifestyle.
🟣 Pedunculated Submucosal Fibroids: Growing into the uterus cavity with a stalk attached to the uterus. Symptoms associated with pedunculated fibroid include pain and pressure, bloating and frequent urination. Acute pain can occur when the fibroids twist on their stalk, cutting off their blood supply.
🟣 Intramural Fibroids: Develop within the muscular wall of the uterus. When this type of fibroid expands, it makes the uterus feel larger and sometimes mistaken for pregnancy or weight gain. As it grows, it can cause excessive menstrual bleeding, which can cause prolonged, heavy menstrual cycles and the passage of large blood clots. Pelvic pain is also another common symptom due to the expanded fibroid pressuring on the surrounding organs. The added pressure can cause secondary symptoms like frequent urination or bowel problems such as constipation.
🟣 Subserosal Fibroids: Develop on the outside of the uterus. The most common symptoms are pelvic pain and abdominal pressure. Depending on the severity, other problem such as frequent urination can accompany this pain and pressure.
🟣 Pedunculated Subserosal Fibroids: Growing from the outside of the uterus into the pelvis with a stalk attached to the uterus. When this type of fibroid continues to grow outward and increasing in size, it may exert additional pressure on the surrounding organs.
See! Each fibroid may lead to different types of symptoms and some are overlapping each other. This explain that it is hard to determine the type of fibroids but just looking at the symptoms you are experiencing.
A woman may have one or more types of fibroids. In fact, it is common for a woman to have multiple fibroid types, which can cause different types of symptoms.
A check up will be good to have a better understanding on the fibroids. Doctor may check on your family & medical history, and confirmed with a ultrasound scanning.
If an ultrasound scanning reveals the presence of fibroids, then the next step is to discuss on the various treatment options.

Treatment Options
If you have fibroids but no symptoms (asymptomatic), you might not need any treatment. Doctor may suggest to monitor annually to see if they have grown.
If you have fibroids and are experiencing mild symptoms, your choices of treatment are:
A) Medicinal
B) Surgery (Conventional or Minimally Invasive)
C) Microwave Ablation
Medicinal treatment may help in lessening the severity of symptoms, but do not eliminate the fibroids. During the treatment, you may experience the signs and symptoms of menopause such as mood swings, weight gain and etc.
However, fibroids tend to grow back and often reach their initial size once the treatment has been stopped.

b) Surgery
If you have fibroids that are causing moderate or severe symptoms, surgery may be the best option. Here are your choices:
Traditional Surgical Procedures:
A major surgery which involve the removal of the whole uterus. When a woman’s fibroids are large, having severe bleeding, is near or past menopause, or does not desire children, she may need this procedure. During the procedure, a big cut will be made on the lower abdomen to take out (remove) the whole uterus. It takes several weeks to recover from a hysterectomy.
Once the uterus is removed, you will not be able to bear children and experience early onset of menopause. In most cases, women with uterine fibroids would choose to keep their ovaries.
This surgery involves the removal of the fibroids only, leaving the uterus in place. Myomectomy can be done in a variety of methods. It can be the conventional way which include cutting on the belly and uterus to remove the fibroid, or minimally invasive approach which will be explained in the next section.
Minimally Invasive Procedures:
It is a keyholes procedure, in which doctor will insert few instruments through small incision on your abdomen to remove the fibroids from the uterus. A camera system will be involved to have a better view of the internal of uterus.
This procedure is an option only if the fibroids are contained inside the uterus (submucosal). Doctor will access and remove the fibroids through vaginal approach.
The Advanced Technology
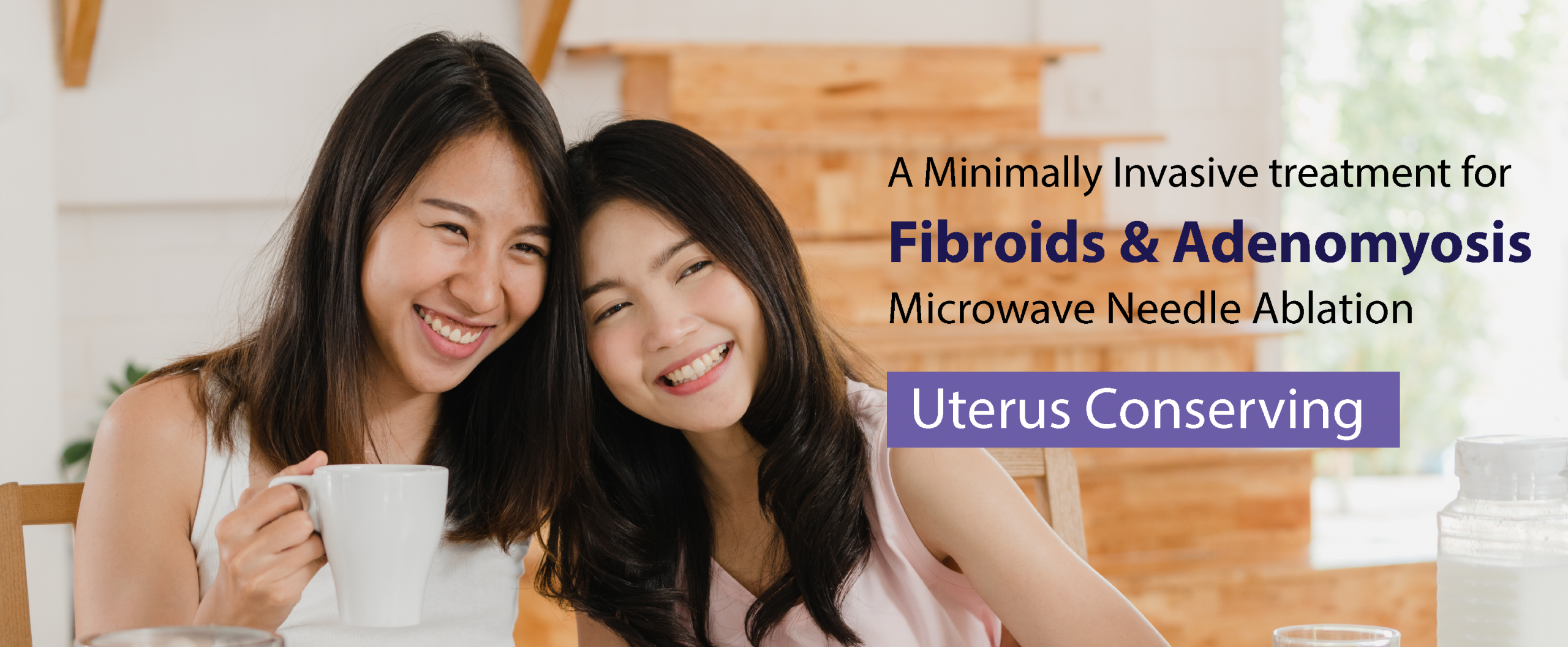
Minimally Invasive Microwave Ablation for Fibroids & Adenomyosis Treatment
An Uterus Conserving Treatment
Microwave Ablation (MWA)
- Without Cutting & Removing Any Tissue
- Go Home The Same Day
- Fast Return To Normal Daily Activities

Did you know?
The same Microwave Ablation Technology has been available in Malaysia since year 2012, widely used by Interventional Radiologists to treat solid cancerous tumours in liver, lung, kidney, adrenal, spleen, bone and others as a Minimally Invasive Cancer Therapy.
How does Microwave Ablation work?
MWA uses electromagnetic waves to produce a tissue heating effect. The oscillation of polar molecules produces frictional heating, ultimately generating tissue coagulation necrosis within the tumour. It destroys and eradicates non-cancerous lesions / adenomyosis by ablating them with thermal ablation.
Mechanism of Microwave Thermal Ablation generates a series of biochemical changes, such as tumour cell dehydration, intracellular protein denaturation, and coagulation that brings the synthesis of tumour cell’s deoxyribonucleic acid (DNA) and protein to a halt. It also destroys the blood supply of the lesion, which results in the necrosis of tumour cells. The treated tumour will be absorbed by body over time, no tissue removal is required.
The Microwave Ablation Procedure
Microwave Ablation treats uterine fibroids and adenomyosis without cutting and removing the uterus. Treatment can be performed by abdominal, vaginal or laparoscopic approach.
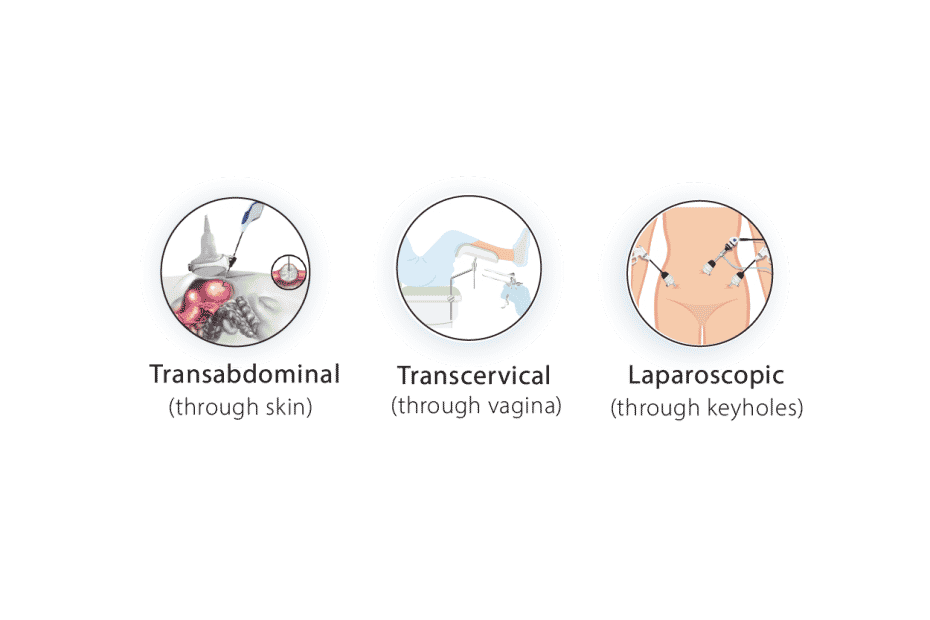
MWA Abdominal Approach

Under real-time ultrasound image guidance, a 1.6mm MWA antenna will be precisely inserted into the targeted area (fibroid).

Microwave heat energy is generated uniformly to kill the tissue inside the fibroid. A 10cm fibroid in diameter can be treated completely in 15 minutes. The treated fibroid will become necrosis, shrink & absorbed by our body over time.

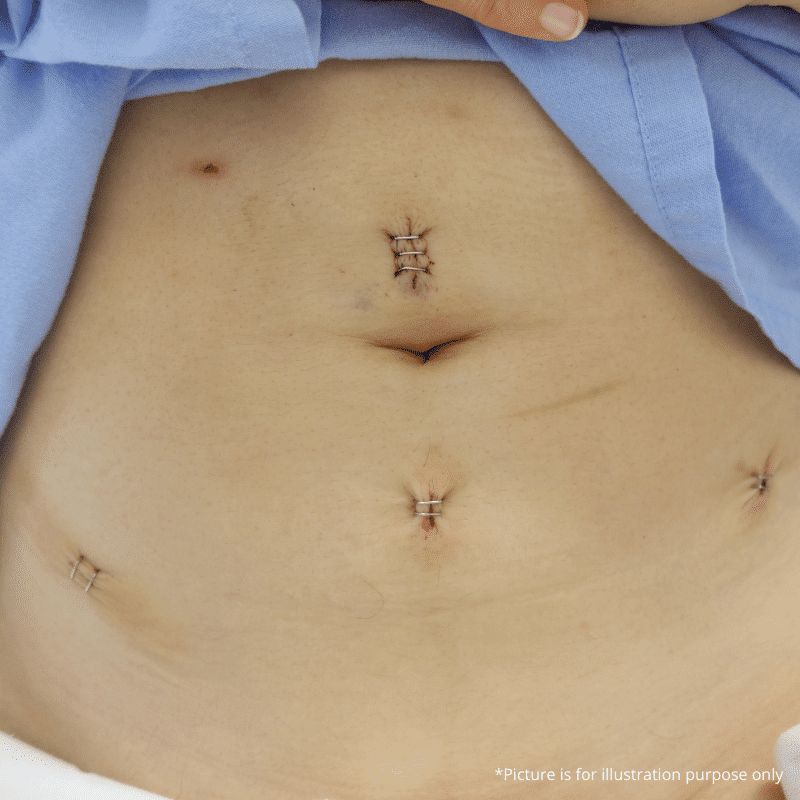
No open wound, no stitch, no scar. Maximum preservation of uterus structure and function.
Why Microwave Ablation?
Precise & Safe
The whole procedure will be precisely monitored by real-time ultrasound imaging to clearly locate the fibroid/adenomyosis and monitor the needle placement as well the ablation progress.
Preserve Your Womb
MWA offers a no-cut, no removal of uterus treatment option for fibroids and adenomyosis. Beneficial for women who have strong desire to preserve their uterus.
Minimally Invasive
- Only a tiny antenna/needle (1.6mm) is inserted into the targeted fibroid
- Excellent cosmetic outcome, no ugly scar
- Almost painless
- Retain uterus structure and function
Fast Treatment Time
- MWA Treatment generally take about 15 minutes for fibroids size of 10cm
- Go home on the same day or next day
- Significant relief of symptoms
- Quick recovery to normal daily activities
In conclusion,
MWA is a minimally-invasive treatment, with benefits as follows:
Almost painless, without cutting or stitching, keeping the uterus intact
Tiny incision, no scarring
Precise treatment, under real-time ultrasound guidance
Go home on the same day or next day
Fast treatment time
Quick recovery
Local Anaesthesia (LA) is possible
Some tips for you!
No clue about what to ask on your next consultation? Here are some suggestive questions for you:

- How many fibroids do I have?
- How big are my fibroid(s)?
- Where is my fibroid(s) located (outer surface, inner surface, or in the wall of the uterus)?
- Is it possible that the fibroid(s) will become bigger?
- How rapidly have they grown (if they were known about already)?
- How will I know if the fibroid(s) is/are increasing in size?
- What kinds of issues might fibroid(s) cause?
- What diagnostics or imaging studies should I use to monitor my fibroids’ growth?
- What are my treatment options if my fibroid(s) becomes a problem?
If you are afraid that you will forget, screenshot and save it to your gallery 😉